Pharmaceutical companies around the world are racing to create a vaccine for SARS-CoV-2 – the virus responsible for COVID-19. Obviously vaccines have been a hot topic over the past few years, but many people aren’t aware of how they work. Hopefully this post can clear this up a bit!
I have a some previous articles that outline what SARS-CoV-2 is and the types of tests we are using now to diagnose COVID-19. In short, there are two types of tests being employed during this pandemic. The first is ‘genetic testing’ that is used to test whether you currently have the virus by looking for its RNA in a sample. The second is ‘antibody testing’ that is used to determine if you’ve previously been exposed to COVID-19 by looking for your antibodies.
Note: This is a long article! I summarize the takeaways at the end.
How does acquired immunity work?
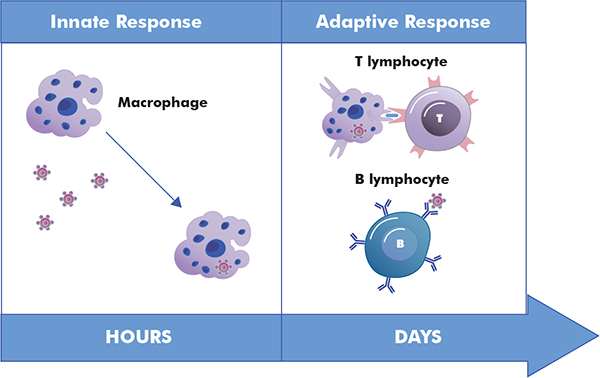
To understand how vaccines work, we first need to think about how the body fights infections. Your immune system has two main ways of keeping you healthy. The first is called innate immunity which refers to defenses your body is born with (ie. physical barriers, ‘defense mechanisms’, and general immune responses). This includes things such as your skin, your tears, and inflammation that keep pathogens out of your body (1). The second is called adaptive or acquired immunity which refers to defenses your body ‘learns’ (2). The adaptive immune system “acquires” the ability to fight off infections after being exposed to bacteria, viruses, or other germs.
First, your body needs to be able to distinguish between self vs. non-self. What this means is your body can tell whether a particle that enters the body belongs to you or it is foreign and potentially harmful. Infectious foreign particles, like bacteria and viruses, make proteins called antigens that give them away to your body. These antigens are what the adaptive immune system uses to train itself and remember that specific pathogen in the future.
What’s involved?
The training process involves a few types of cells:
- Macrophages: These cells are types of white blood cells that are able to swallow germs and pathogens, as well as dead cells, and digest them! After they digest them, they leave the antigens behind so other immune cells can recognize and learn from them. These are present in the innate and acquired immune response.
- Antibodies: Not a type of cell, but a protein. Antibodies are produced by B-cells in response to a new antigen. Once made, antibodies are specific to the antigen and can recognize that antigen again in the future.
- B-cells: Made in the bone marrow, these cells are a type of white blood cell normally found in the lymphatic system (which works closely with the immune system). B-cells express antibodies on their surface. When a B-cell encounters an antigen it recognizes, it prompts the cell to ‘mature’ and change into a ‘specialized’ B-cell.
- Memory B-cell: Basically a copy of the parent B-cell that expresses the same membrane-bound antibodies to continue the job.
- Effector B-cell: Produces more antibodies and secretes them according to the specific antigen the parent B-cell recognized. These secreted antibodies now work to recognize the pathogens infecting the body.
- T-cells: Also formed in the bone marrow, these cells are also a type of white blood cell. T-cells have receptors on them that are also able to recognize antigens. However, the antigens they recognize must be attached to receptors on infected cells or macrophages. Like B-cells, T-cells will differentiate after identifying an antigen.
- Helper T-cells: Coordinate other cells to come attack the infected cells.
- Killer T-cells: Release toxins to kill the infected cells.
When the body encounters a pathogen for the first time, it can take a few days for all these cells to go to work recognizing and making antibodies for it. But, after fighting the pathogen for the first time, the immune system keeps around a few T-cells and Memory B-cells so that it can quickly take care of that infection if you get exposed again.
What do vaccines do?
Okay! Sorry that previous section was a bit long, but its important to understand how your body actually responds to a bacteria or viral pathogen.
Vaccines work by imitating an infection and kicking your adaptive immune system into gear (3). When your immune system identifies the vaccine, it can make antibodies in the same way as if it were a real infection. Then, when you do encounter the real thing, your body already knows how to fight it. The key here however, is it is an imitation and not the real thing. This is why getting a vaccine does not make you sick. There are different types of vaccines that we use to imitate these infections and they are usually broken up into two categories:

Attenuate (live) vaccines
Attenuated vaccines utilize a version of the living bacteria or virus that is weakened so that it won’t cause an infection in the body (4). These obviously work very well because they are as close as you can get to having the actual infection. Most often these attenuated vaccines are made by growing up the bacterium or virus in cell culture and over time selecting for less virulent, or less disease causing, strains (5). For example, the measles vaccine was created after almost 10 years of passing the virus until the wild virus was turned into an attenuated vaccine (6).
However, due to the time it takes and the unpredictable nature of this method, other methods are now being incorporated to create vaccines. There are also some cons to using live attenuated vaccines. First, attenuated vaccines are hard to store and transport. Because they are a living organism, things like light and heat can damage the organism and make it ineffective. Second, live attenuated vaccines are meant to reproduce within the body. But, sometimes this can mean the organism can revert over time back to the more virulent strain, causing disease. Finally, those with suppressed immune systems may have reactions to live vaccines since their body is not able to respond in the normal way. Because of these things, live attenuated vaccines are no longer as common and are more highly regulated for safety.
Inactivated vaccines
In contrast, inactivated vaccines are non-living vaccines (6). These are usually made by growing up the bacteria or virus and then inactivating them with either heat or chemicals. Once inactivated, the organism is not able to replicate in the body and instead, a dose of the antigen for that pathogen is administered in the vaccine injection. Because they don’t replicate, these vaccines always require the administration of multiple doses to give the body time to acquire its immunity. However, these inactivated viruses are much safer for those immunocompromised because they are unable to cause infection.
Inactivated viruses can contain the whole inactivated organism or “fractional” parts of the organism which include protein-based vaccines or polysaccharide based vaccines. An example of a whole inactivated organism vaccine is the rabies vaccine.

In protein based fractional vaccines, the vaccine may contain subunit products of the organisms or toxoids (7). Subunits, like the name suggests, contain only parts of the virus or bacteria including things like the specific antigens of the organism. An example of a subunit vaccine is the influenza vaccine. Toxoid vaccines are designed against bacteria that produce toxins when they enter the body. Here, the vaccine contains weakened toxins that will train the immune system to fight off the natural toxin. An example of a toxoid vaccine is tetanus.
Finally, conjugate or polysaccharide vaccines are a type of subunit vaccine that contains polysaccharides from the surface of some organisms. Polysaccharides are long chains of carbohydrate molecules that comprise the surface capsule of many bacteria. Conjugate vaccines contain a polysaccharide molecule joined to a carrier protein. In polysaccharide vaccines, there is only the carbohydrate. Examples of these vaccines include vaccines for pneumococcal and meningococcal diseases (6).
With advances in technology, we are also seeing new recombinant vaccines. These types of vaccines rely on genetic engineering to produce antigens for an organism. This is often done by inserting part of the pathogen’s genetic material into a non-harmful host cell such as yeast. The host cell then produces the antigen for the original pathogen which can be used as a vaccine. An example of a recombinant vaccine is the Hepatitis B vaccine.
What is the SARS-CoV-2 vaccine progress?
Now that you know more about how vaccines work and what types there are, we can look at some of the vaccines in development for COVID-19. However, this in no way will be an all inclusive list. There are hundreds of companies all over the world working toward developing a SARS-CoV-2 vaccine. Not only this, but in most countries, especially the U.S., there is a thorough pipeline of testing that all new drugs must go through before being available on the market. Drug testing is a whole other topic on its own, but I will be putting out another article in the future on that. For now, I have linked some resources if you are interested about this process (8, 9, 10).

Some of the top companies you may have heard about in the news include Pfizer, Moderna Therapeutics, Inovio Pharmaceuticals, Sinovac, and Johnson & Johnson. This resource has a good list of current companies working on drug and vaccine discovery (at the time I am writing this article)(11). The WHO also published a draft list of vaccine candidates at the end of April (12). All of these are in different stages of the development process (13).
- BioNTech in collaboration with Pfizer – BNT-162 mRNA vaccine
- BioNTech is a Germany based company that has teamed up with Pfizer in designing a vaccine for SARS-CoV-2 (13). Currently they are in phase I and II clinical testing in Germany. Their vaccine is a messenger RNA (mRNA) vaccine (14). mRNA is responsible for bringing the information from the DNA to the rest of the cell so it can carry out a function. Here, the mRNA would code for the COVID-19 antigen, causing the body to produce more antigen and then develop immunity for it. This would be considered a subunit vaccine.
- NIAID in collaboration with Moderna Therapeutics – mRNA-1273
- Similarly to above, the National Institute of Allergy and Infectious Diseases (NIAID) has teamed up with Moderna Therapeutics to design a vaccine. They are also designing an mRNA vaccine that has just entered into phase II clinical trials (15).
- Inovio Pharmaceuticals – INO-4800
- Inovio is currently designing a DNA-based vaccine that is in phase I clinical trials. A DNA vaccine would work by genetically engineering the viral DNA coding for the antigen. The immune system would then react by producing antibodies. This would also be considered a subunit vaccine.
- Sinovac Biotech in collaboration with Dynavax – Inactivated coronavirus candidate with vaccine adjuvant CpG 1018
- Sinovac and Dynavax are combining their efforts using multiple ways to create a COVID-19 vaccine. First, Sinovac used a chemically inactivated version of SARS-CoV-2 and showed protection in Rhesus monkeys (16). Second, Dynavax hopes to combine their developed adjuvant CpG 1018 to elicit an increased vaccine immune response (17). This vaccine has currently entered phase II human trials.
Like I mentioned, these are just a few of the many vaccines in development for COVID-19. Resources like the WHO, Science, and Nature have all been reporting up to date stories on current vaccine development. The time it takes to get a drug or vaccine to market is long and tedious, but is for the health of everyone. Hopefully this information can help you to understand what some of the vaccine candidates are, and how vaccines work within the body.
Takeaways
- Vaccines work by stimulating your adaptive or acquired immune response. This means that next time you come into contact with that pathogen, you will know how to fight it.
- Antibodies, memory B-cells, and T-cells help your body remember the pathogen after you’ve been infected or been vaccinated
- There are two main groups of vaccines: Live (attenuated) vaccines and inactivated vaccines.
- Live vaccines have greater risks than inactivated vaccines because they are able to reproduce in the body.
- Inactivated vaccines can contain whole or part of the organism they are trying to protect you from.
- There are hundred of SARS-CoV-2 vaccines in development around the world in different stages of clinical trials.
Overall, I hope this gave you some information on how viruses work and where we are with developing a COVID-19 vaccine. Development takes time and lots of testing to be sure that the drug that is made public is safe and effective.
Some Helpful Sources:
- Nature, five questions as trials begin – here
- Technology Networks, Drug Development Process – here
- WHO, draft COVID-19 vaccine candidates – here
- Biopharma Trend, list of vaccines – here



Leave a Comment